Today, I would like to introduce the challenging three-branch orthotopic reconstruction TEVAR surgery brought by the team of Professor Chang Guangqi/Li Zilun/Wu Weibin from the First Affiliated Hospital of Sun Yat-sen University. The patient had a large aortic arch pseudoaneurysm, located in the anterior wall of the aortic arch, and the proximal end of the lesion had involved the root of the left common carotid artery, and the proximal anchoring area was obviously insufficient. Moreover, the distance between the three branches of the supraarch is very short, and the brachiocephalic artery is only 1.5 mm away from the left common carotid artery, so it is necessary to continue to extend the anchoring area proximally and reconstruct the three branches of the supraarch artery. So what surgical options are available to treat this patient safely and effectively? Which stent graft is available to effectively seal and isolate the lesion? And what techniques will be used to perform suprabowular reconstruction with a long-term prognostic outcome? The team of Prof. Chang Guangqi/Li Zilun/Wu Weibin used HuamaiTech thoracic aortic stent graft and only 0.018" CTO guidewire soft head to efficiently complete the reconstruction of the left common carotid artery and the left subclavian artery through in-situ fenestration technology, and completed the reconstruction of the brachiocephalic artery through chimney technology, and the postoperative effect of the patient was good.
Description
Gender: Male
Age: 65 years old
History of present illness: more than 2 weeks ago, he was admitted to the hospital for "dizziness and vomiting", and the aortic arch penetrated ulcer with wall thrombosis. He came to the hospital for further treatment and diagnosis of aortic arch pseudoaneurysm, aortic arch ulcer, and abdominal aortic thrombosis.
Past medical history: generally in good health, denial of hypertension, diabetes, appendectomy 17 years ago.
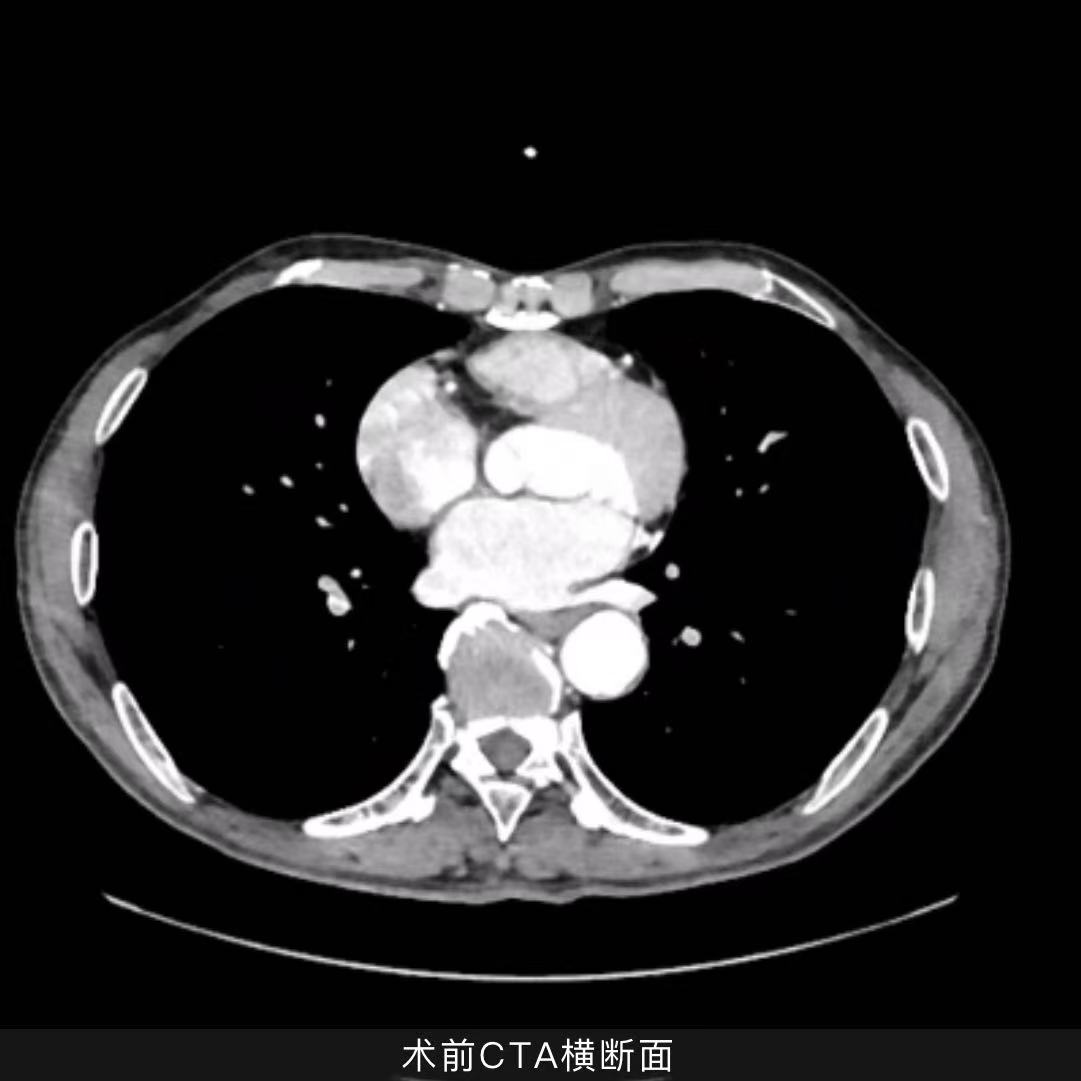
CTA details: aortic arch pseudoaneurysm, the lesion is located in the anterior wall of the arch, the size of the aneurysm is 37.6*32.9*22.1mm, the proximal end has involved the proximal end of the root of the left common carotid artery (LCCA), the brachiocephalic trunk (IA) is only 1.5mm away from the LCCA, and the LCCA is only 4mm away from the left subclavian artery (LSA). The diameter of the aorta at the neck of the aneurysm is 34 mm.

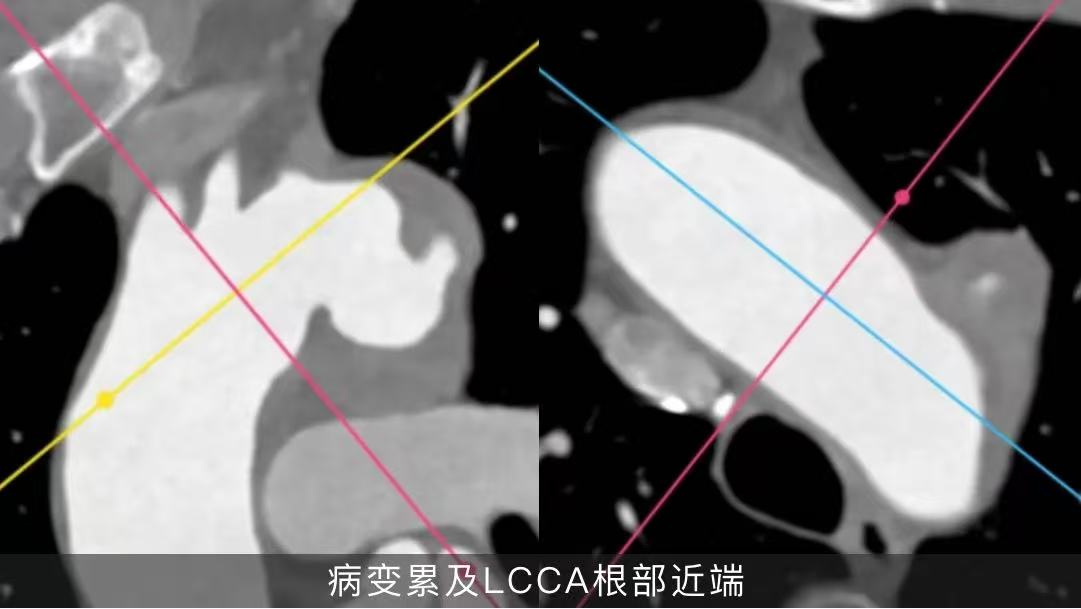
Difficult to treat
•Aortic arch pseudoaneurysm is located in the anterior wall of the arch, the proximal end of the lesion has involved the LCCA root, the proximal anchoring area is obviously insufficient, and the distance between the three branches of the supraarch is very short, so it is necessary to extend the anchoring area proximally to reconstruct the three branches of the supraarch artery.
•Pseudoaneurysms have large lesions and high requirements for proximal sealing of thoracic aortic stent grafts.
•LSA is at an acute angle to the aortic arch, which brings difficulties to the control of the in-situ fenestration angle during surgery, and it is difficult to open the window with common stent grafts on the market.
•Aortic arch lesions with mural thrombosis are severe, and gentle maneuvering should be done.
Surgical protocol strategy
Option 1
Thoracic aortic stent graft endovascular repair + supraarch three-branch chimney technique: the surgical operation is relatively simple, but the risk of occlusion of the left common neck and left subclavian artery is relatively large, the risk of endoleakage is high, and the medium and long-term results are not good.
Option II
Endovascular repair of thoracic aortic stent graft under external fenestration: pseudoaneurysm closure has a good effect and can retain the original hemodynamic characteristics, but the three branches of the supraarch are all externally fenestrated, which is complicated to operate, and the stent needs to be modified according to the measurement results before surgery, which takes a long time; Intraoperative hyperselection windows require precise alignment, which is a high risk.
Option III
Endovascular repair of thoracic aortic stent graft + brachiocephalic dry chimney technique + left common carotid artery and left subclavian artery in situ fenestration: the lesion closure effect is good, the hemodynamics of the three branches of the supraarch can be preserved, and there is no need for preoperative stent modification. However, the in-situ fenestration of traditional aortic stent grafts has high requirements for interventional devices, and special membrane permeation instruments such as in-situ fenestration needles, lasers, and biopsy needles are required.
Considering the medium- and long-term treatment effect and the simplicity of intraoperative operation, and after comprehensive evaluation, the team of Prof. Chang Guangqi/Li Zilun/Wu Weibin again selected HuamaiTech thoracic aortic stent graft for endovascular repair, and reconstructed the left common carotid artery and left subclavian artery by in-situ fenestration technique.
Surgical procedure
Considering the medium- and long-term treatment effect and the simplicity of intraoperative operation, and after comprehensive evaluation, the team of Prof. Chang Guangqi/Li Zilun/Wu Weibin again selected HuamaiTech thoracic aortic stent graft for endovascular repair, and reconstructed the left common carotid artery and left subclavian artery by in-situ fenestration technique.
Endovascular repair of thoracic aortic pseudoaneurysm + brachiocephalic trunk artery chimney stent reconstruction + left common carotid artery in situ fenestrated stent reconstruction + left subclavian artery in situ fenestrated stent reconstruction
01.After successful anesthesia, the patient was placed in a supine position, routinely disinfected and clothed, punctured the bilateral femoral arteries, and placed a 6F short sheath. Two vascular closures were embedded in the right femoral artery and the 8F sheath was replaced.
02. Bilateral brachial artery puncture, each with a 7F long sheath. The left brachial artery sheath tip is placed above the LSA opening, and the right brachial artery sheath tip exceeds the brachiocephalic trunk artery opening by about 2 cm into the ascending aorta.
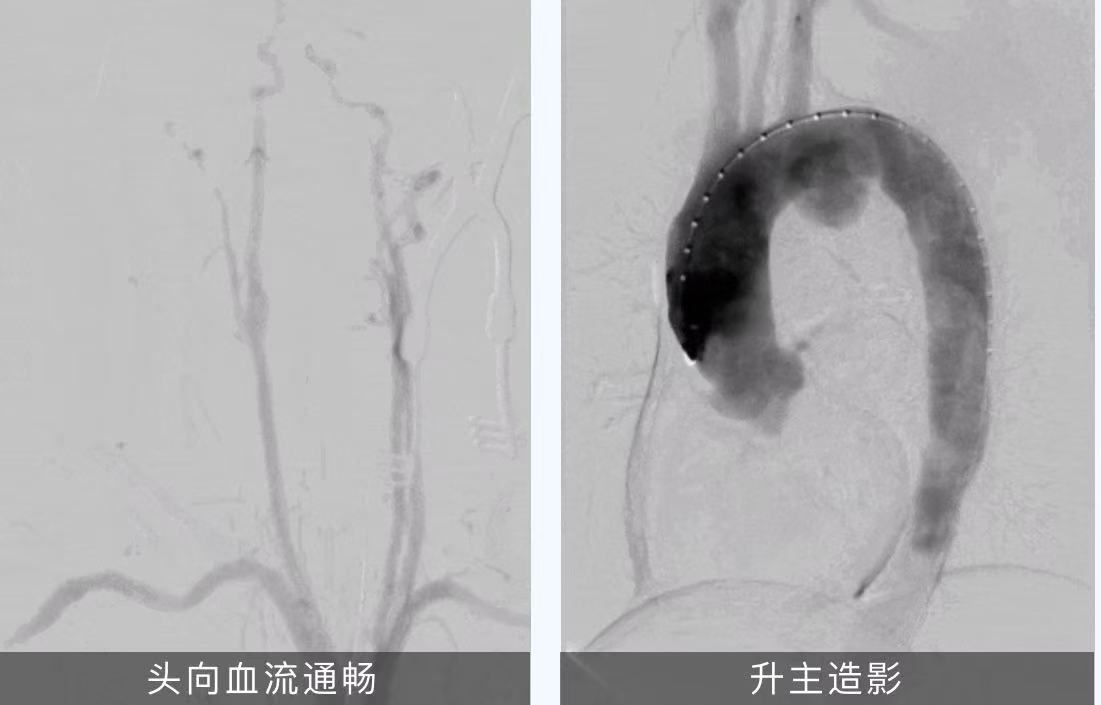
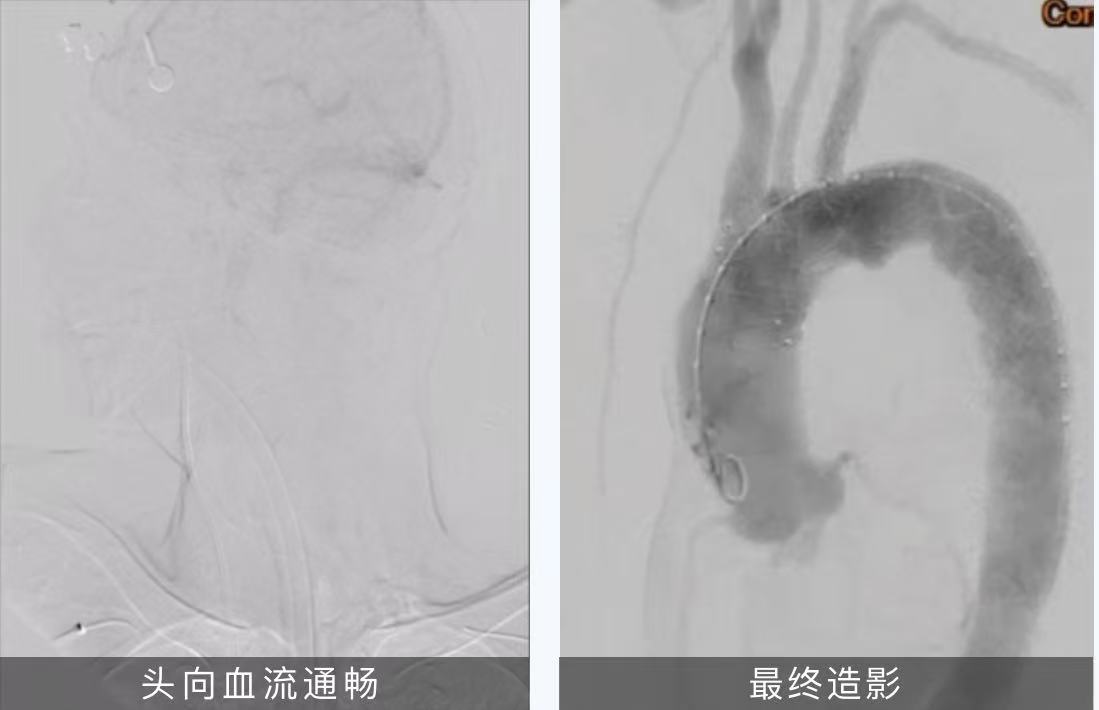
03.Aortic arch angiography: bilateral common carotid artery blood flow is smooth, LSA blood flow is smooth, LVA is patency advantage, and Willis ring is intact. A pseudoaneurysm can be seen anterior to the minor curvature of the aortic arch at the level of the LSA opening, and the extent of the aneurysm sac is close to that of LCCA
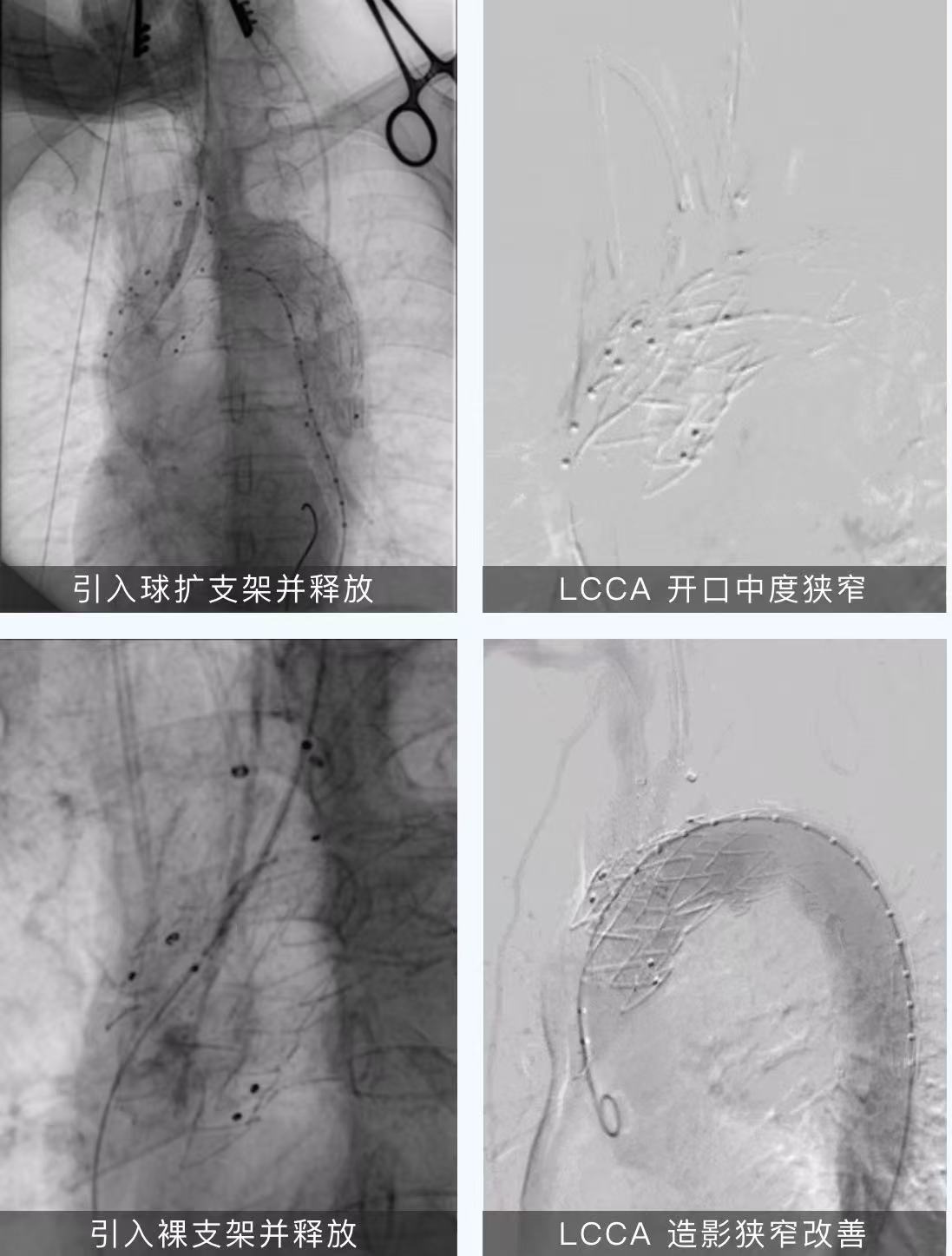
04. The IA long sheath is pre-imported with 14-60 GPS bare brackets, and the black loach is introduced into the left neck to the main standby, and the Huamai PTBS3834180 is introduced, covering about 2/3 of the IA opening, and the easy-to-open window is located at the LCCA and LSA opening. Slowly release the 2-3 stents, and after reconfirming the positioning, quickly release the remaining part and then release the bare bare bare tip. The IA chimney technique releases the bare stent with the bare stent front edge of the bare stent at the tip of the flat Huamai covered stent. The imaging showed that the stent was accurately positioned, the lesion was completely isolated, no obvious endoleakage was found, the IA stent was in good shape, the blood flow was smooth, the LCCA was developed, and the reconstruction took 1.5 minutes.
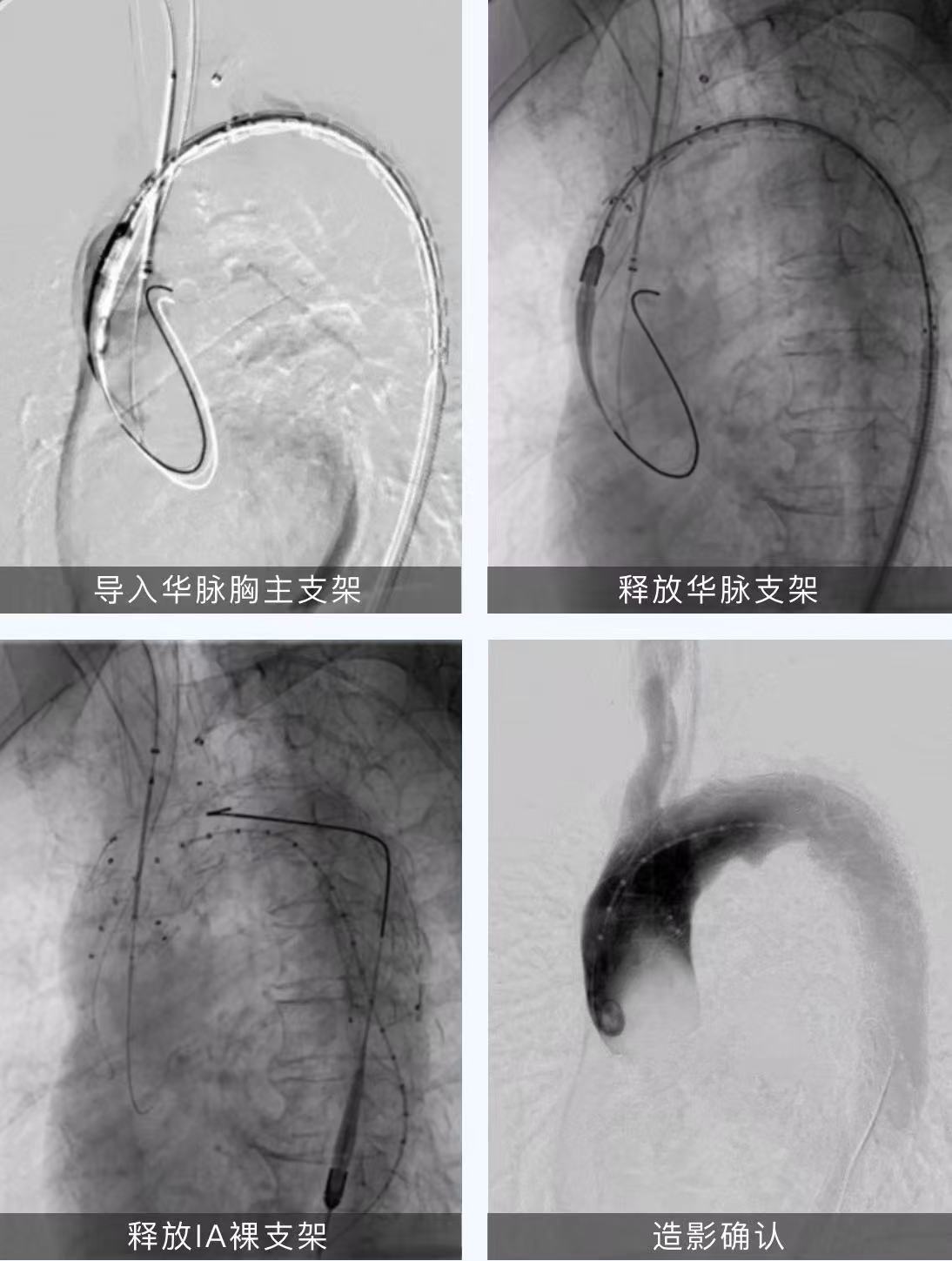
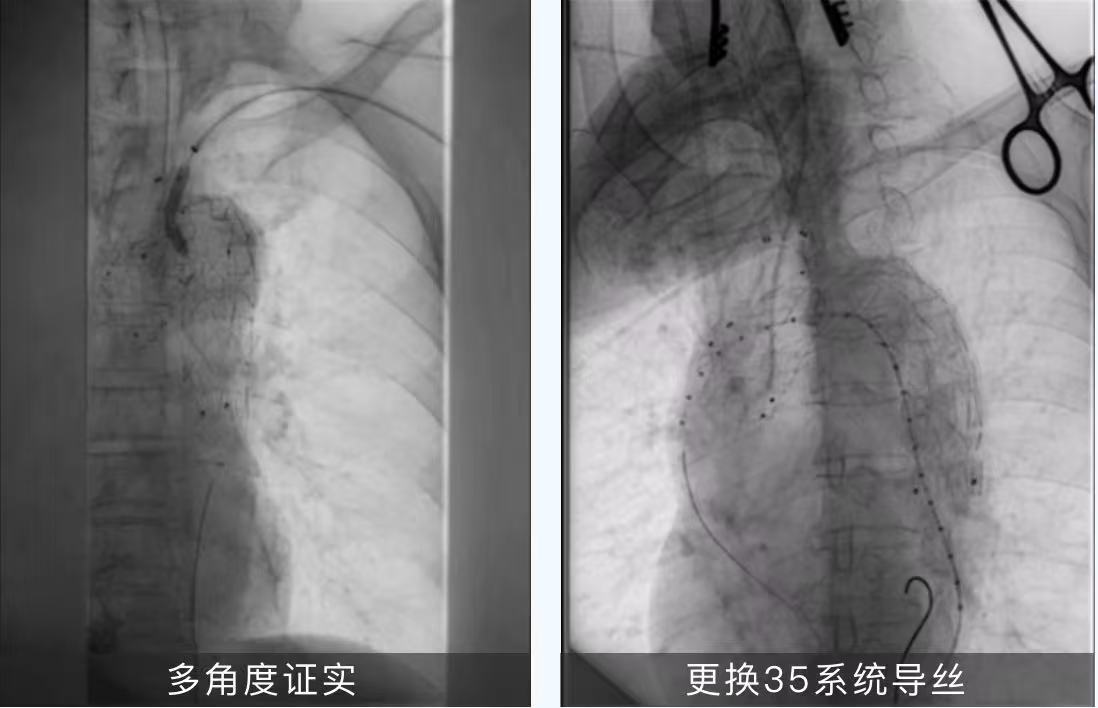
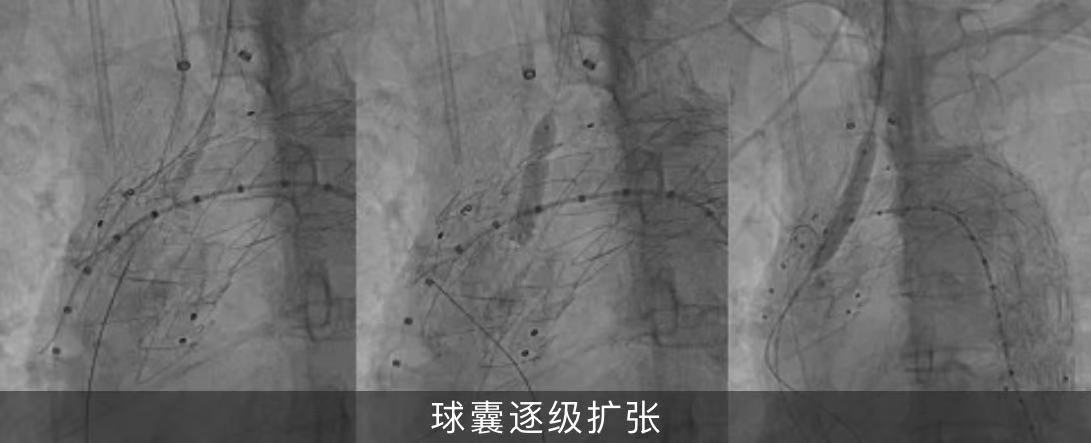
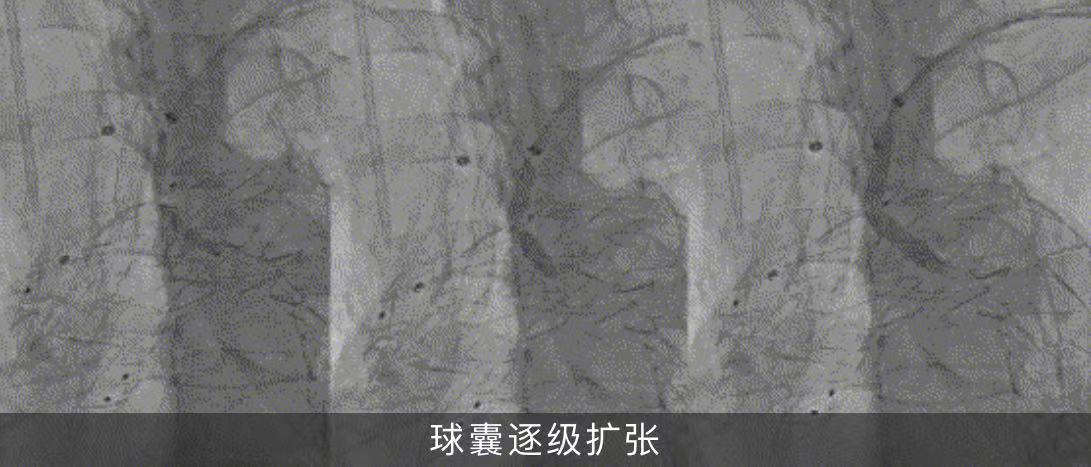
05. The Fusmart adjustable bending catheter was introduced into the LCCA sheath, and the tip of the catheter was adjusted to the stent graft at the aortic arch, and the 250T Connect guidewire was sent along the catheter to successfully permeabilize the membrane, and the multi-angle fluoroscopy confirmed the successful rupture of the membrane, and the 4-30mm Sterling balloon, 6-30mm Mustang, and 8-40mm Mustang balloons were used to dilate the rupture and open the window step by step.

06. Through the balloon sheath technique, the 8-37mm Lifstream splamshell expander stent was inserted through the aortic fenestration site, the tip end entered the stent graft about 20mm and then released, the LCCA opening was still moderately stenotic on the imaging, the 8-40mm Mustang balloon continued to expand backwards, and the 8-40mm Absolute bare stent lining was introduced, and the reconstruction took 15 minutes.
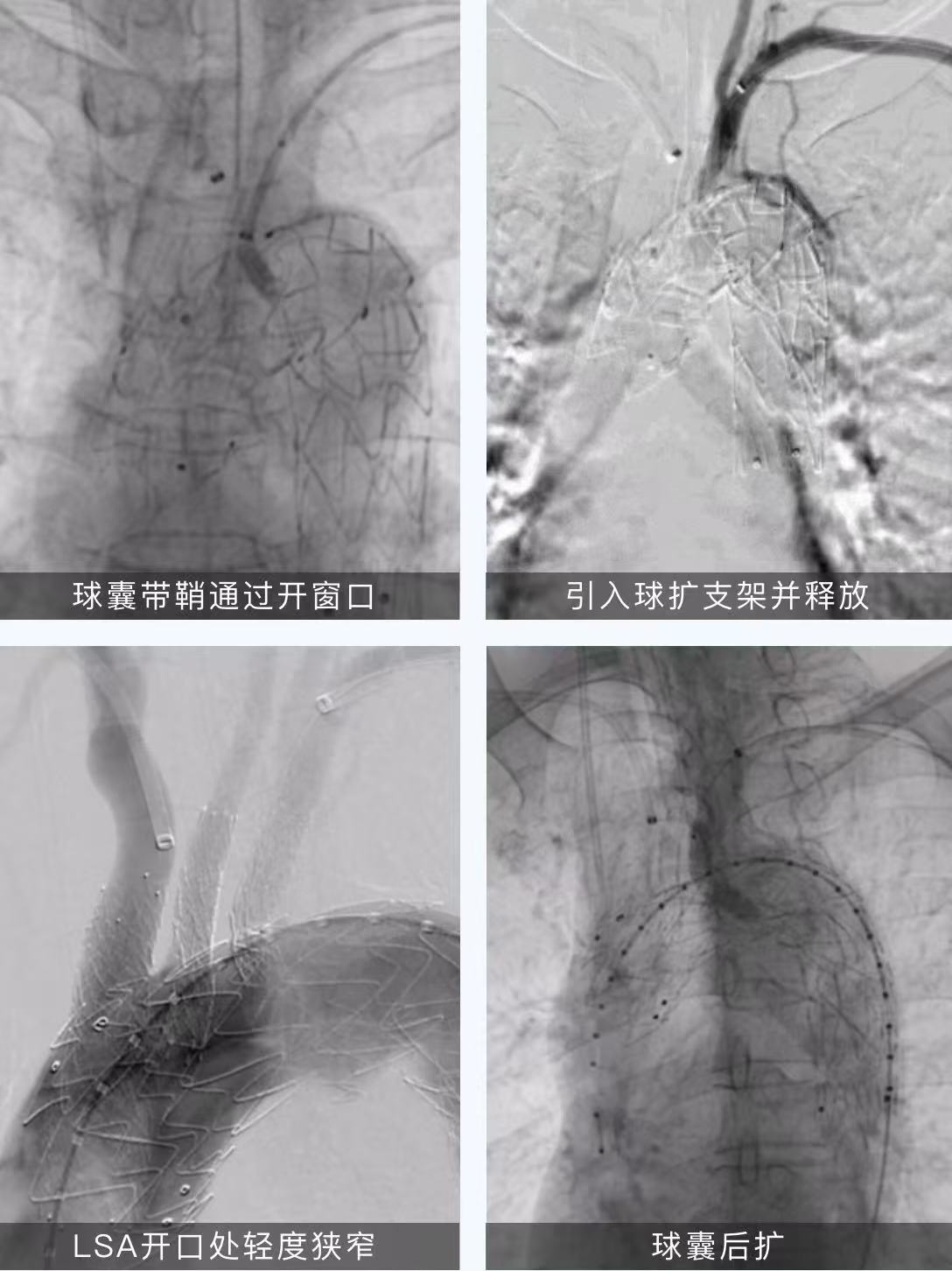
07. A Fusmart adjustable bending catheter was introduced into the left brachial artery sheath, and the catheter tip was adjusted and multi-angle fluoroscopy was confirmed to be the correct stent graft at the aortic arch, and a 250T Connect guidewire was sent along the catheter to successfully permeate the membrane. A 3-40mm Saber balloon was successfully fed along the left brachial artery for dilation, followed by a 4-30mm, 5-30mm Saber balloon, and a 6-40mm Mustang balloon.

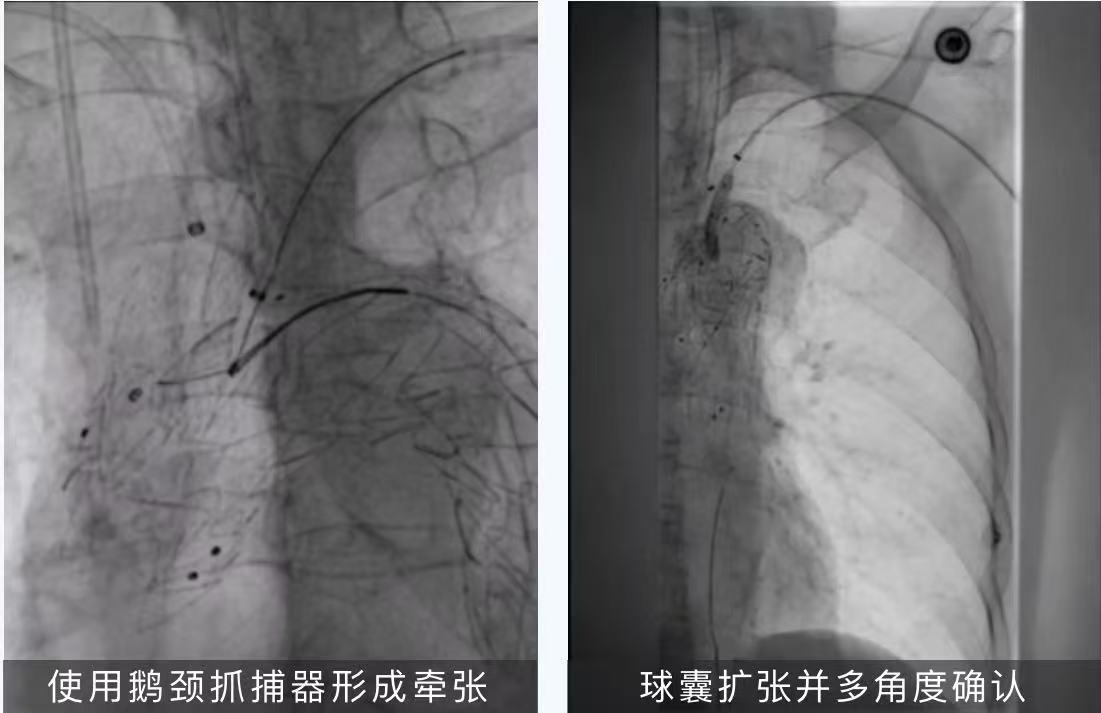
08. Balloon sheath technology is used to insert a 9-38mm Lifstream spherical expansion stent through the aortic fenestration, and the tip end is released after entering the stent graft about 10mm, and a 10-60mm Evercross balloon is used to expand it backwards. So far, the reconstruction of IA, LCCA and LSA has been completed.
09.The final imaging showed that the position and shape of the stents were good, the thoracic aortic pseudoaneurysm was completely isolated, there was no cerebral infarction, the innominate artery, the left common carotid artery, and the left subclavian artery had smooth blood flow, and there was no obvious endoleakage.
10. Remove all guidewire catheters and sheaths, close the puncture point, apply pressure bandage, fully stop bleeding, close the left neck incision layer by layer, and complete the operation.
Pre-discharge review versus preoperative examination

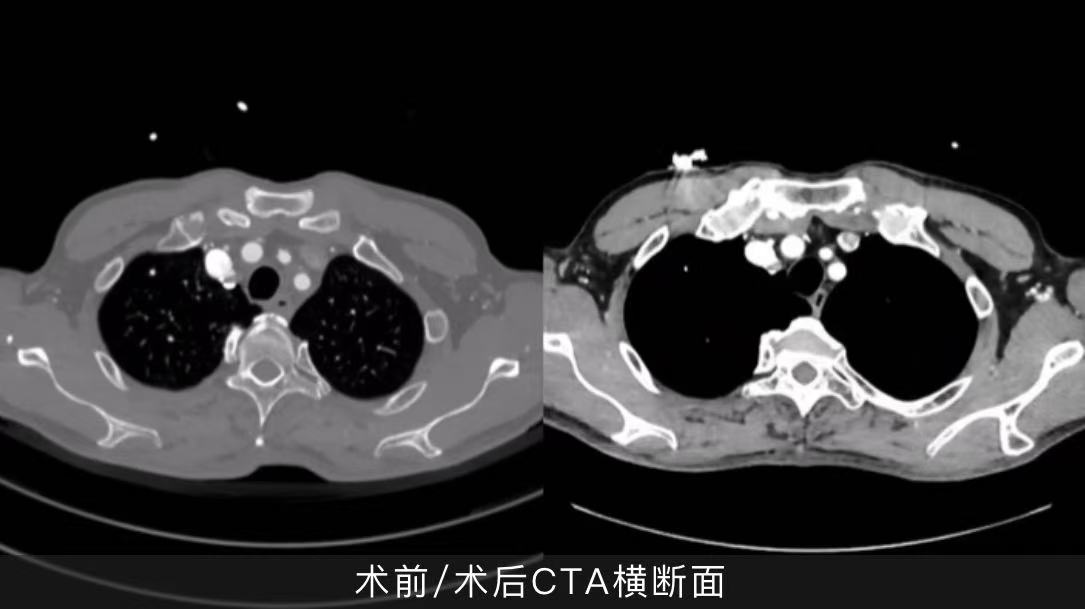
The postoperative recovery was good, there was no cerebral infarction and cerebral ischemia, the aortic arch pseudoaneurysm was completely isolated, the branch stent was patency and the shape was good.
Summary of case experience
In the case shared this time, the aortic arch pseudoaneurysm is large, located in the anterior wall of the aortic arch, the proximal end of the lesion has involved the root of the left common carotid artery, and the distance between the three branches of the supraarch is very short, so it is necessary to continue to expand the anchoring area proximally and reconstruct the three branches of the supraarch artery. From the evaluation of the surgical plan to the selection of surgical methods and stent grafts, the team of Prof. Chang Guangqi/Li Zilun/Wu Weibin chose Huamai Tyco's thoracic aortic stent graft to reconstruct a single branch artery by in-situ fenestration technology after accumulating many cases of experience in reconstructing a single branch artery using Huamai Tech's thoracic aortic stent graft again, and only used a 0.018" 250T CTO guidewire to easily break the membrane, and efficiently completed the reconstruction of the left common carotid artery and the left subclavian artery. The short time to block blood flow in the critical branch arteries of the supraarch does not require special cerebral perfusion techniques, simplifying the surgical procedure. The proximal positioning of the thoracic aortic stent graft is accurate, the lamination at the window is easy to penetrate and expand, and the membrane can be broken instantaneously with only the CTO guidewire soft head, the balloon expansion opening process is simple, safe and reliable, the shape is good after stent implantation, the lesion sealing effect is good, there is no membrane leakage, the effect is clear, and the prognosis of the patient is good. In the end, the effect of the reconstruction of the three branches on the bow in this case was in line with the expectation of preoperative planning.