Today, the editor will share with you the case of the treatment of thoracic aortic aneurysm by the team of Professor Lu Qingsheng of the First Affiliated Hospital of the Naval Medical University. Welcome everyone to read, learn, exchange and discuss!
Case Profile
Age : 71
Gender : Male
Chief complaint : Chest and waist pain for 7 days
History of present illness:
The patient had tear-like pain in the chest and waist for no obvious reason 7 days ago, no syncope, fever, no nausea, vomiting, no abdominal distension, abdominal pain, no hematuria, bloody stool, no relief of symptoms after rest, and was treated in a local hospital, and the abdominal and chest CTA examination showed aortic arch dissection and local aneurysm dilation; Left common iliac artery ulcer with wall thrombus
Anamnesis and personal history: History of hypertension for more than 20 years, up to 160/90mmHg plain blood control.
INVESTIGATIONS:
CTA of the whole aorta suggests aortic archaneurysmal dilation, and small local ulcers may be present. Intramural hematoma at the beginning of the descending aorta, upper abdominal aorta, and left common iliac artery.

Initial diagnosis:
1. Thoracic aortic aneurysm
2. Hypertension grade 2 (very high risk)
Surgical Options:
Pseudo-aortics + thoracic aortic aneurysm endovascular isolation + left common cervical and left subclavian artery stenting + right common femoral artery endarterectomy.
Difficult cases
1. The patient has eccentric aortic arch aneurysm, high risk of rupture and bleeding, meets the indications for surgery, and the open surgery is traumatic, and the patient and his family refuse to open the operation, so endovascular repair is chosen;
2. The aneurysm is located at the distal end of the left subclavian artery, close to the opening, and there is a problem of insufficient distance between the anchoring area. After the fenestration stent is released, in order to avoid stent displacement and torsion, the left subclavian artery and left common carotid artery are intended to be stent fixed;
3. Brachiocephalic trunk, left common carotid artery, and left subclavian artery are located in the ascending aorta, which belongs to type III. aortic arch classification, and there is a problem that it is difficult to overselect the branch artery after the release of the fenestration stent;
4. The aneurysm is located in the aortic arch, the branch artery is located in the ascending aorta, and the proximal end of the stent will be located in the ascending aorta, and there are possible complications such as aortic dissection and arterial leakage;
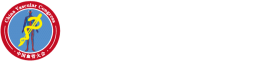
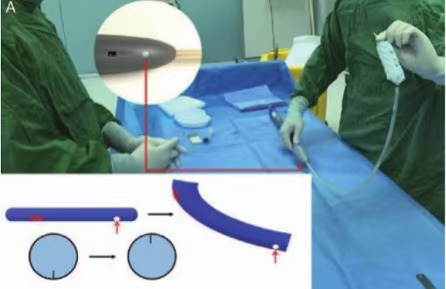
▲External fenestration technique--- Accurate fenestration technique depends on accurate preoperative measurements
• Preoperative measurement using Endosize software. The anatomical and morphological characteristics of the aortic arch and its branch arteries were measured by 1mm CTA imaging. Factors measured include the diameter of the proximal and distal stent anchoring area, the optimal angle at which the three branches are deployed intraoperatively, the length of the major bend of the aortic arch, the diameter of the branch artery, the distance between the openings at the major bend of the branch artery, and the representation of the position of the ostium of each branch in the clockwise direction.
• Rotation is not allowed while repairing the fenestration bracket. The following principles should be followed during the process of sheathing the sheath: (1) do not shorten the distance between any components; (2) Do not rotate any parts; (3) Do not move the scaffold graft forward with the outer sheath; (4) Do not release the device after opening the tip.
•Small fenestration of bridging stents prevents stent migration and reduces the risk of branch artery stenosis or occlusion and endoleakage. The guidewire should be advanced within the fenestration stent and through the fenestration into the target branch artery. The diameter of the bridging stent should be equal to or slightly greater than the diameter of the fenestration 28, and it is recommended that the bridging stent be inserted into the aorta by approximately 1 cm. Postdilation is required when there are signs of stenosis or occlusion within the bridging stent.
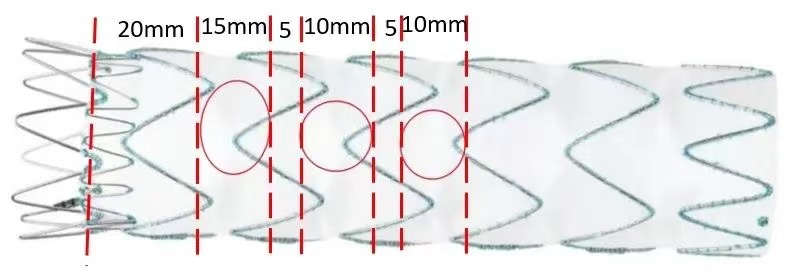
▲Space inversion technology
The white dot of the foregrip remains at 6 o'clock (red arrow) during the advancement of the delivery system, and the opening coaxial to the white dot mark on the foregrip reverses to the 12 o'clock direction as it crosses the greater curve side of the aortic arch.
Surgical plan
•Anesthesia : General anesthesia
•Surgical approach: Right femoral artery, left brachial artery, left carotid artery incision
• Implant : Aortic stent 42-200, triple fenestration; left carotid artery Fluenecy 10-60; Left subclavian artery Fluency 12-60
Surgical procedure
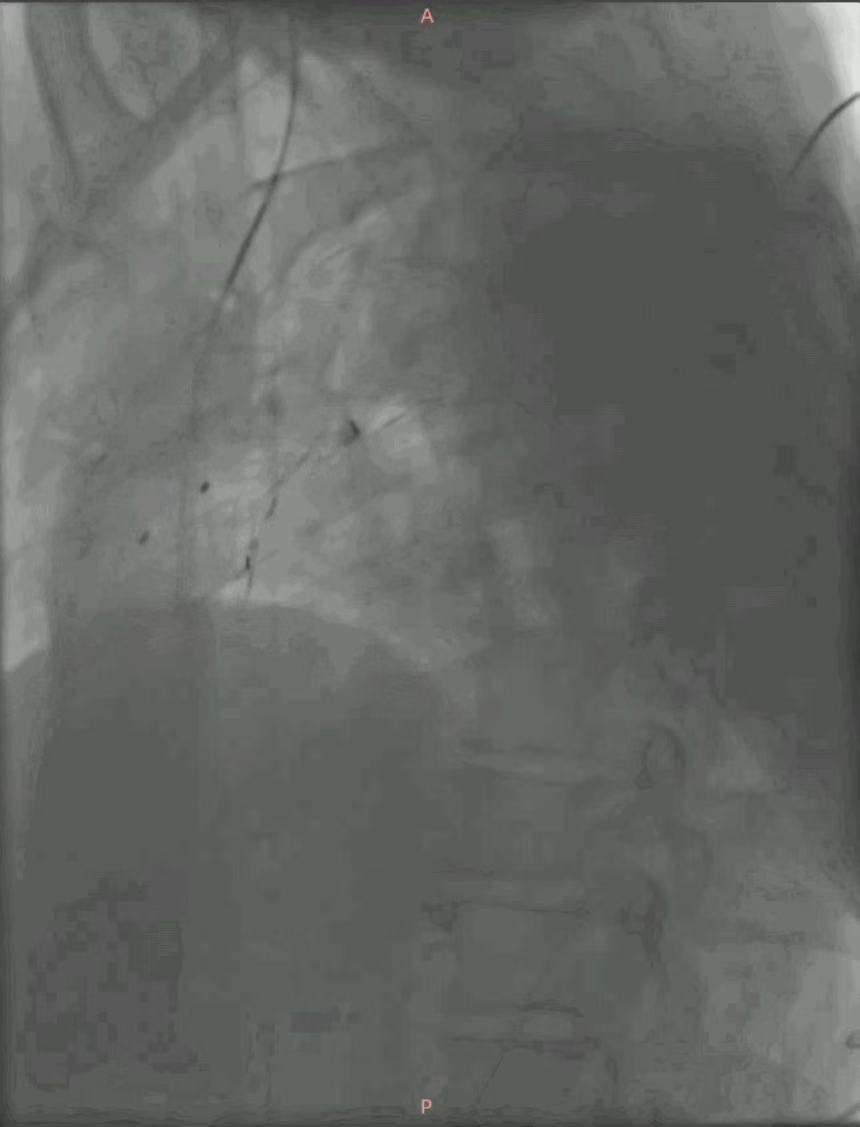
Porcine tail catheter angiography shows an aortic arch aneurysm, consistent with preoperative testing.
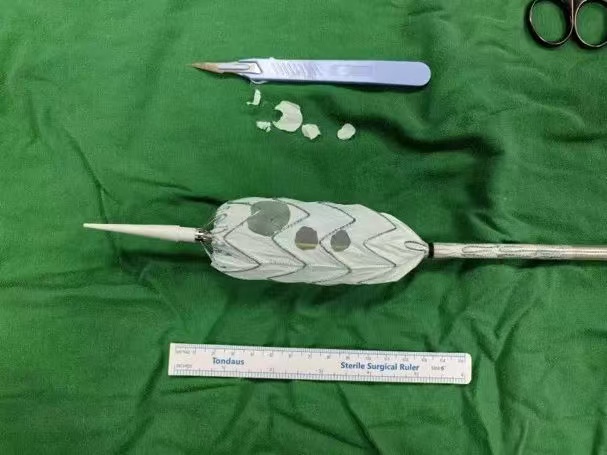
The thoracic aortic stent (42-200) was released on the table and recovered after fenestration.
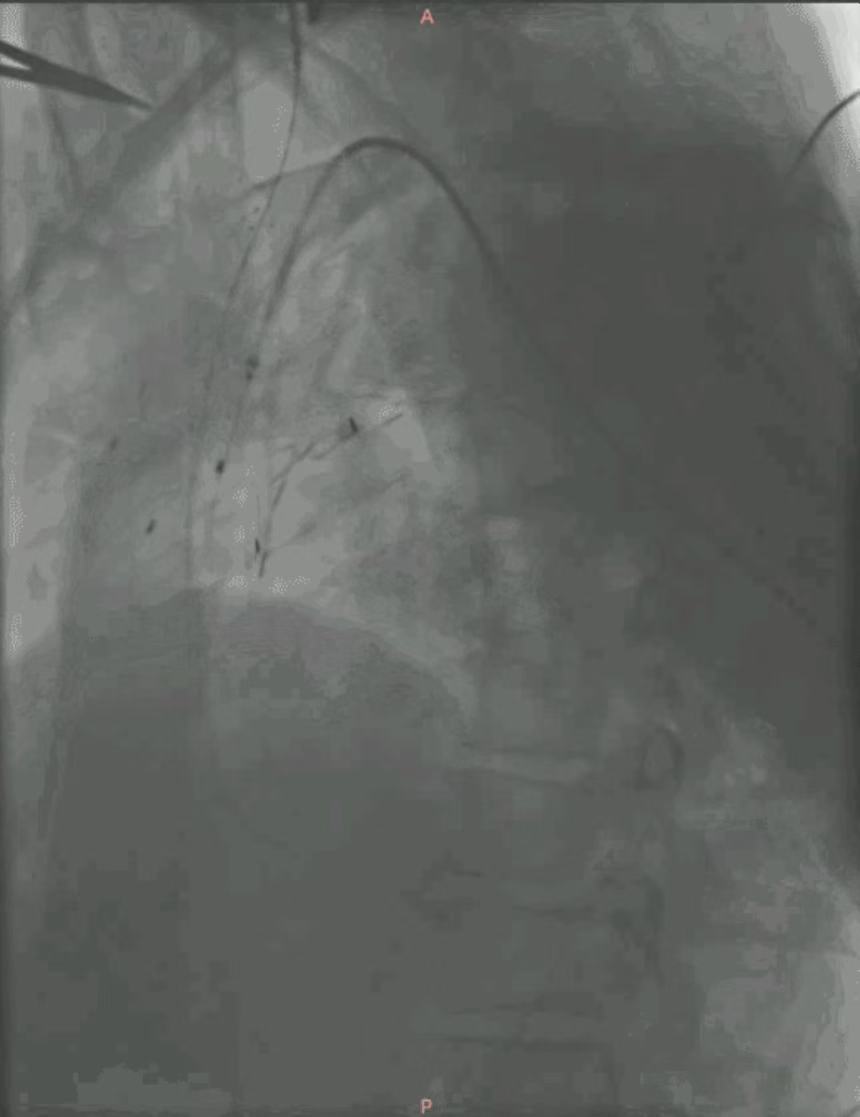
Release after thoracic aortic stent positioning:

The guidewire was combined with a single-bent catheter to overselect the left carotid artery fenestration, and after confirmation, a Fluency stent (10x60mm) was introduced for positioning and release.
The left subclavian artery fenestration was overselected by the same method, and the Fluency stent (ard, 12x60mm) was introduced for positioning and release after confirmation.
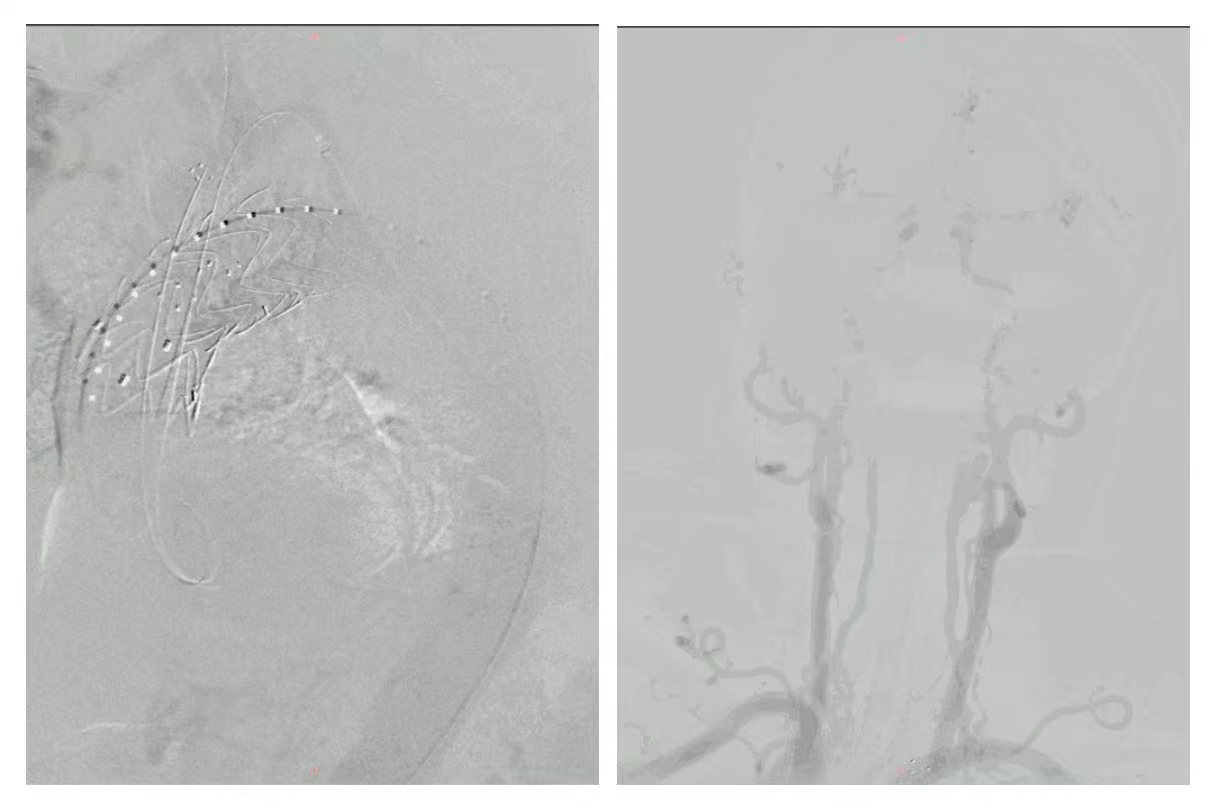
Angiography showed that the thoracic aortic aneurysm was completely isolated without endoleak, and the brachiocephalic artery, left common carotid artery, and left subclavian artery were unobstructed. Neurogram showed good intracranial blood supply and no filling defects.
Postoperative situation
1. Pay attention to the activity of limbs, muscle strength and nerve signs after surgery, and be alert to complications such as craniocerebral artery embolism.
2. Postoperative anticoagulation therapy to prevent acute thrombosis of stents.
3. Observe whether there is bleeding in the neck incision and airway management to avoid subcutaneous hematoma affecting breathing
4. Postoperative ECG monitoring and blood pressure control (systolic blood pressure about 120mmHg)
5. The right lower limb and left upper limb were straightened and immobilized for 24 hours, and the distal arterial pulse was observed to be vigilant for distal ischemic events.
6. Postoperative cefuroxime to prevent stent graft infection and dexamethasone to prevent postoperative inflammatory reaction.
Summary and experience
1. The patient's aneurysm involves the three branches of the arch, and the surgical operation has the risk of acute cerebral infarction caused by plaque detachment, and the three branches are fenestrated during the operation, and the left common carotid artery and left subclavian artery are stent placed, and it is necessary to be vigilant against complications such as stent thrombosis, which affects the blood supply of the corresponding branches. Therefore, it is necessary to complete the brain MRI and other related examinations before surgery to evaluate the risk of cerebral infarction during and after surgery, and at the same time, it is necessary to fully inform the patient's family of the risk of cerebral infarction.
2. Compared with open surgery, endoluminal isolation has the advantages of less trauma, less bleeding, fast recovery, and low perioperative mortality, and at the same time, in vitro prefenestration can significantly reduce the ischemia time of the three branches of the arch, but it puts forward very high requirements for accurate and careful measurement before surgery.
3. Be alert to complications such as post-endovascular repair syndrome (PERS), graft infection, acute thrombosis, and cardiovascular and cerebrovascular accidents.