Today, the editor will share with you the case sharing of the application of Venovo venous stent in iliac vein compression syndrome combined with varicose veins of the lower limbs brought by the team of Professor Wuren Batu of the Right Front Banner People's Hospital of Xing'an Mengke. Welcome everyone to read, share, exchange and discuss!
Case presentation
1.Case status
Age: 57 years old
Gender: Female
Chief complaint: Tortuous dilation of superficial veins in both lower extremities for 20 years, exacerbation with superficial vein thrombosis for 4 years.
Physical examination:
both lower limbs are of equal length, and a large number of superficial veins are tortuous on the medial side of the lower legs of both lower limbs, and the left area is long. Localized pigmentation of the skin of the right anterior tibial region and medial malleolus with rupture of the anterior tibial skin. Mild pitting edema can be palpated in the right ankle area, normal skin temperature and skin tone in both lower extremities, tenderness in both femoral triangles (-), gastrocnemius squeeze test (-), Homans' sign (-), good pulsation of femoral and popliteal arteries and dorsum pedis and posterior tibial arteries in both lower extremities, normal superficial sensation in both lower extremities, muscle strength grade V, and normal muscle tone.
Anamnesis:
In the past, he was in good health, and 3 years ago he underwent multiple foam sclerotherapy injections in private clinics for superficial varicose veins of the lower limbs, and the results were not good. 27 years after birth control with no history of allergies.
Risk factor: Standing for a long time (barber).
Diagnosis: bilateral varicose veins of the lower extremity, intermuscular vein thrombosis of the left lower extremity, chronic venous insufficiency of the right lower extremity (C5 grade), chronic venous insufficiency of the left lower extremity (C4 grade).
Preoperative evaluation
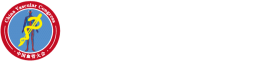
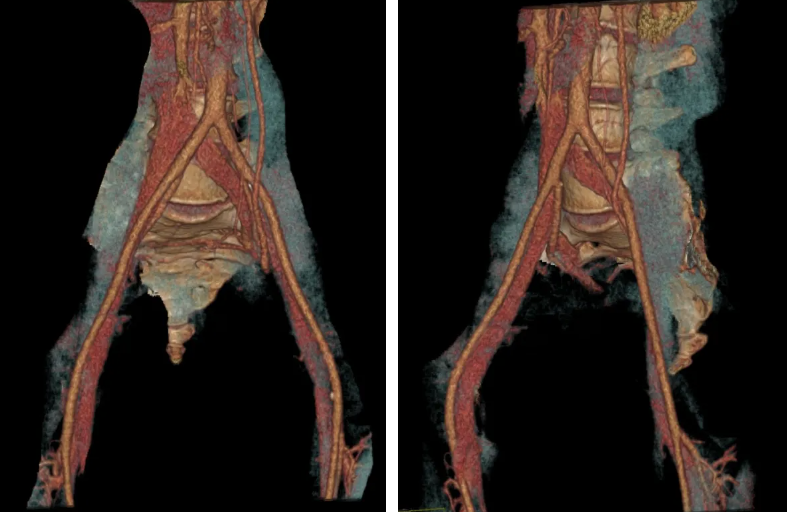
(1) Preoperative lower abdominal status and enhanced CT three-dimensional reconstruction: showed severe stenosis near occlusion at the beginning of the left common iliac vein, and obvious left-to-right shunt of the internal iliac vein.

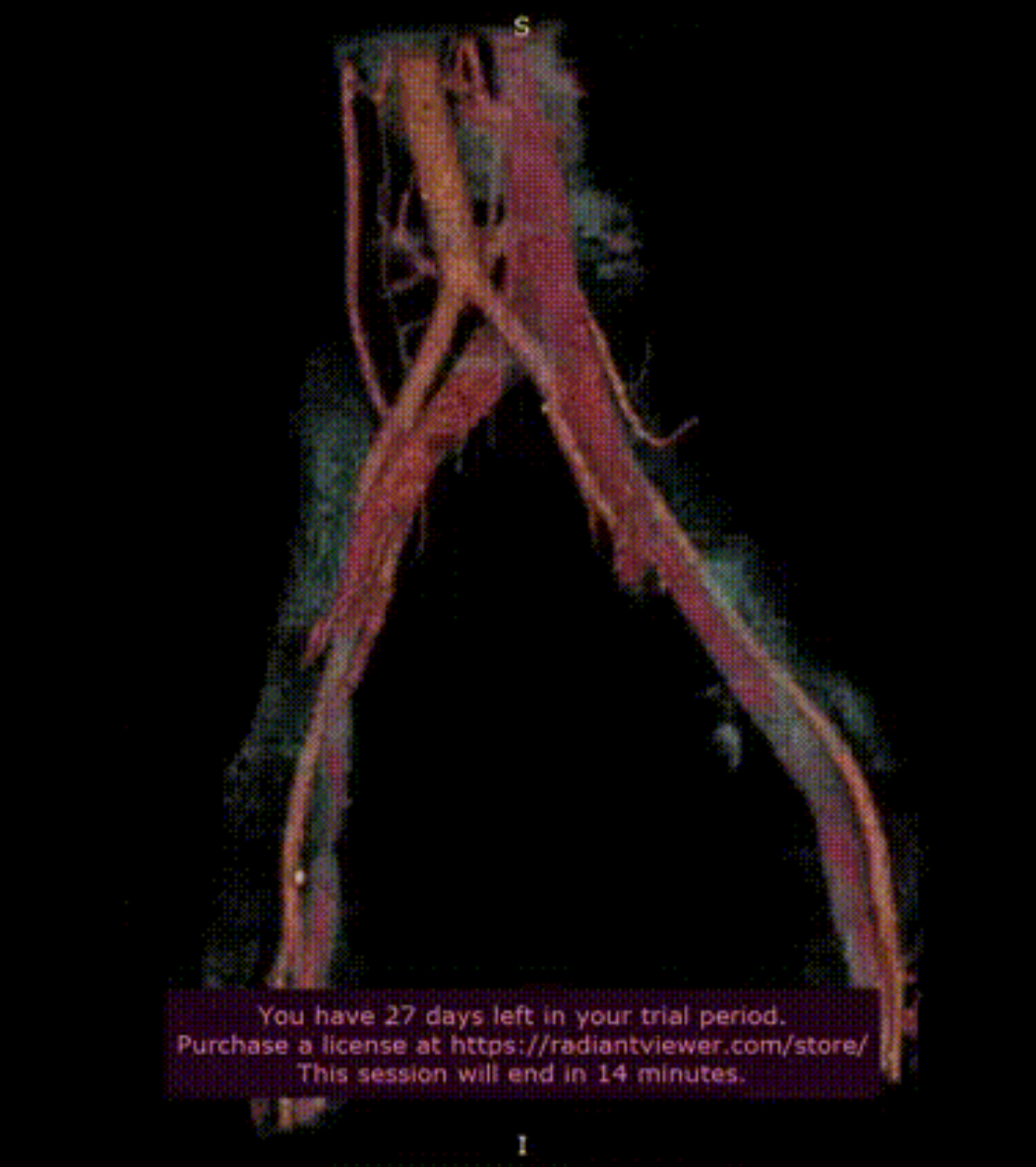
(2) Preoperative cis-venography of the lower extremities:
Preoperative imaging showed severe stenosis at the beginning of the left common iliac vein, obvious left-to-right shunt of the internal iliac vein, and slow blood return in the iliac vein.
Details of the case
2.Characteristics of the case
He had a history of standing for a long time in the past, the main clinical manifestations of symptoms and physical examination of lower extremity venous return disorders, and the two-way examination of preoperative DSA and CT three-dimensional reconstruction verified that the left common iliac vein was significantly narrowed and compressed, the diagnosis of left Cockett syndrome was clear, and the indication for iliac vein stent implantation was clear.
Surgical protocol analysis
3. Treatment plan and strategy
Access opening policy:
(1) Left iliac vein balloon dilation stent implantation.
(2) Left saphenous vein high ligation and peeling + punctate decortication of sub-knee varicose veins.
(3) Approach: In the supine position, a 1cm incision was made along the preoperative marker in the main trunk of the great saphenous vein in the left lower limb in the arcurelus ovale, and the main trunk of the great saphenous vein was separated and exposed, and the proximal end of the main trunk of the great saphenous vein was punctured, and the 10F vascular sheath was indwelled.
(4) The guidewire catheter was turned over the mountain, and bilateral iliac vein and inferior vena cava angiography were performed through the sheath and catheter to confirm the iliac vein infusion location.
(5) Left iliac vein balloon stent implantation.
4.Proposed use of surgical instruments and drugs
Instrument selection plan: 10F vascular sheath, 0.035 loach with hard guidewire or Supra Core 35 guidewire, 12mm, 14mm diameter balloon, 16mm*60mm Venovo venous stent.
Surgical procedure
5. Surgical process
1) Anterolateral angiography to clarify the stenosis again
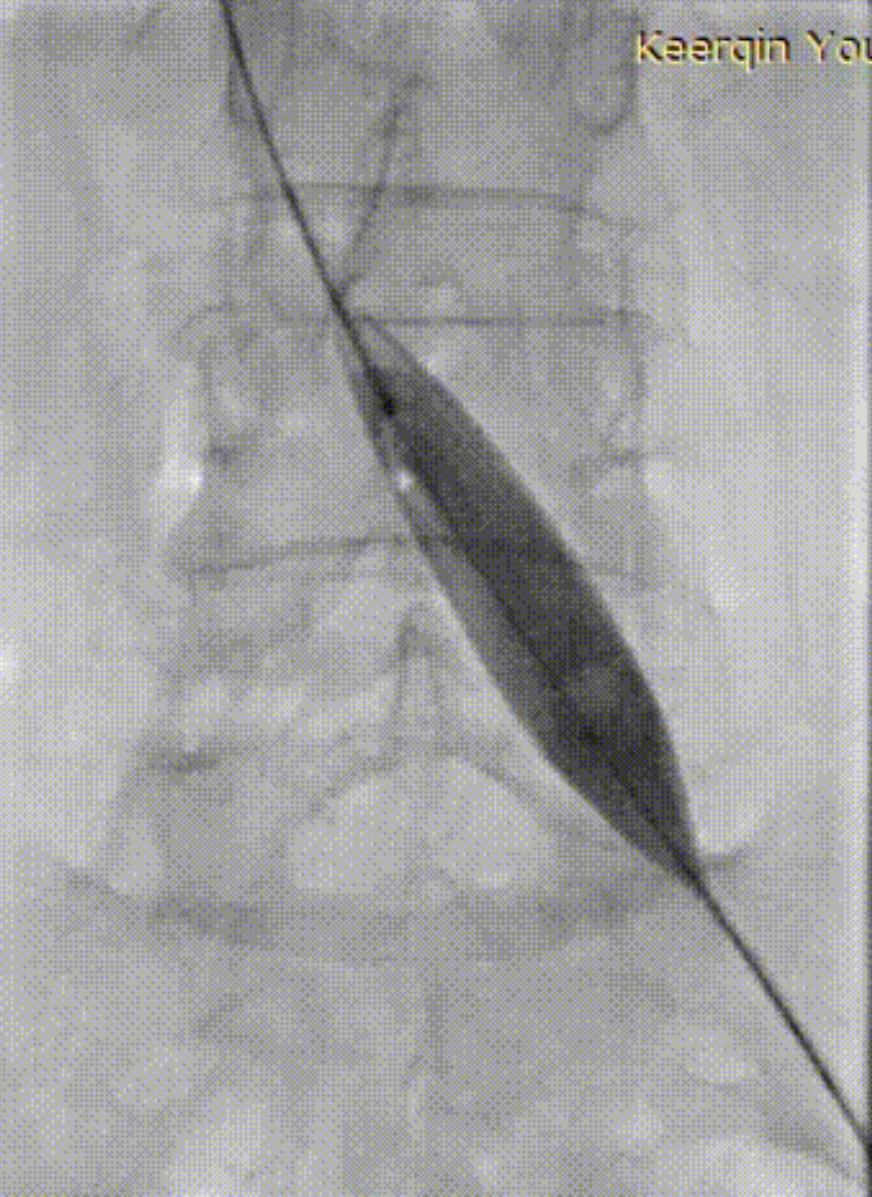
2) The 14mm diameter balloon was pre-expanded, and the "waist" formation of the middle and anterior segment of the balloon was visible.
3) Vertebral artery catheter turning mountain angiography to clarify the location of the biiliac vein inflow
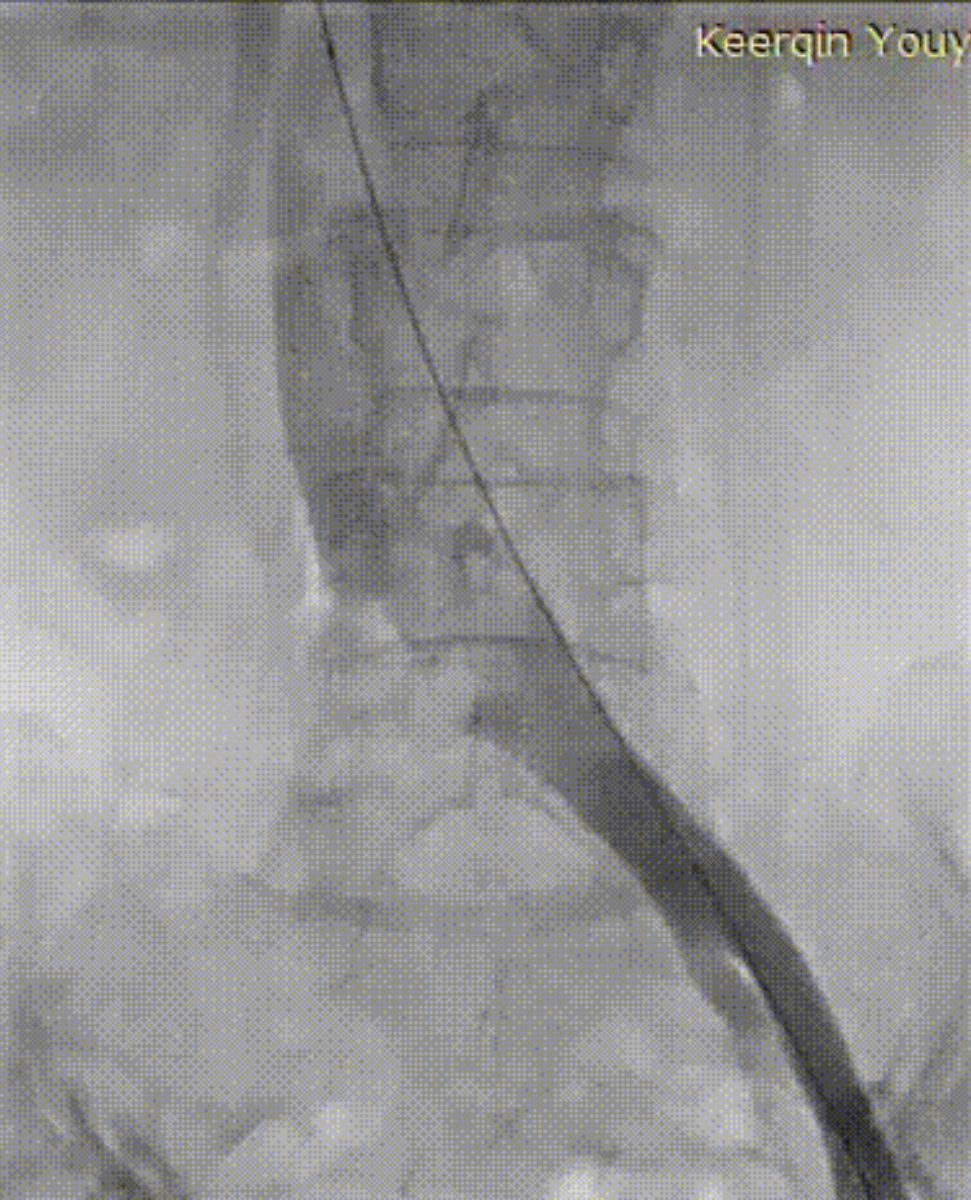
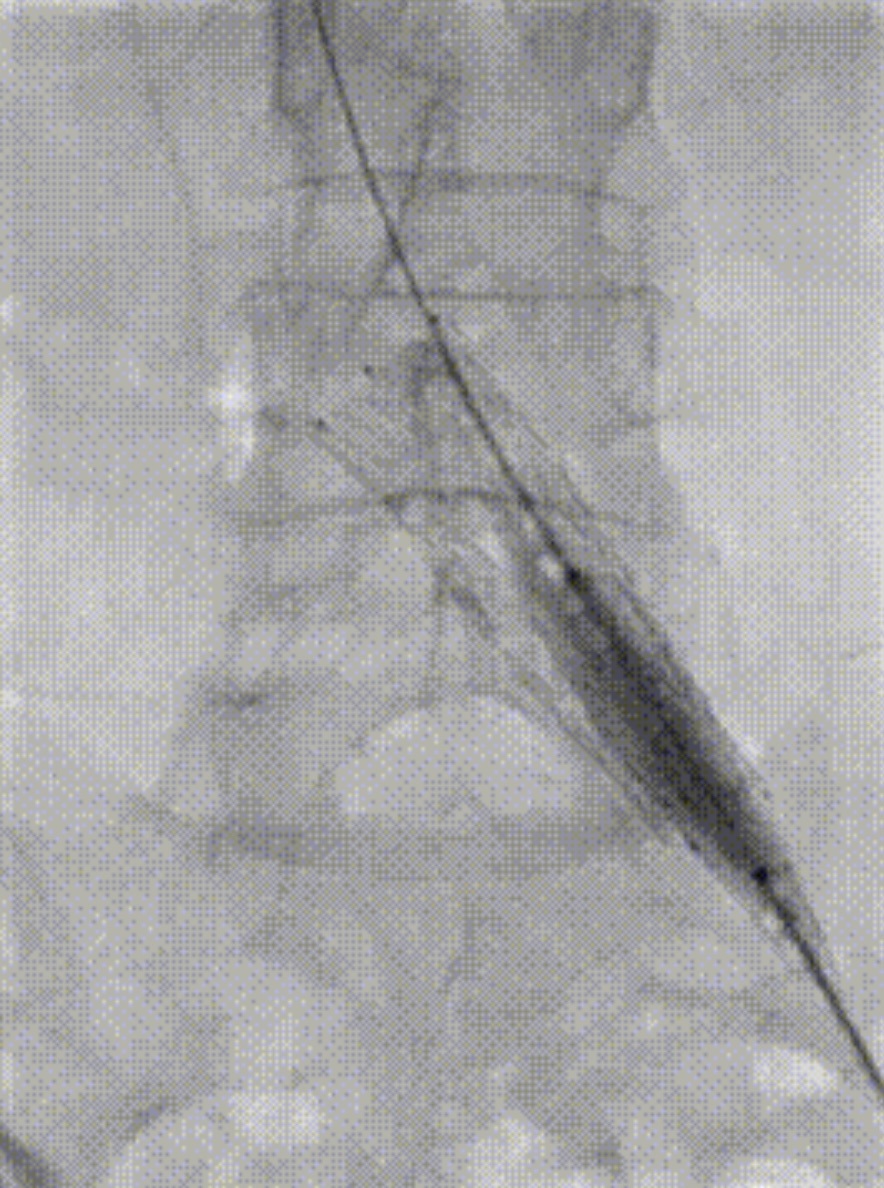
4) After the position is clarified, the 16mm*60mm Venovo Static Stent should be used for positioning and release.

5) After the stent is released, post-expansion is given, and the stent form is fully opened.
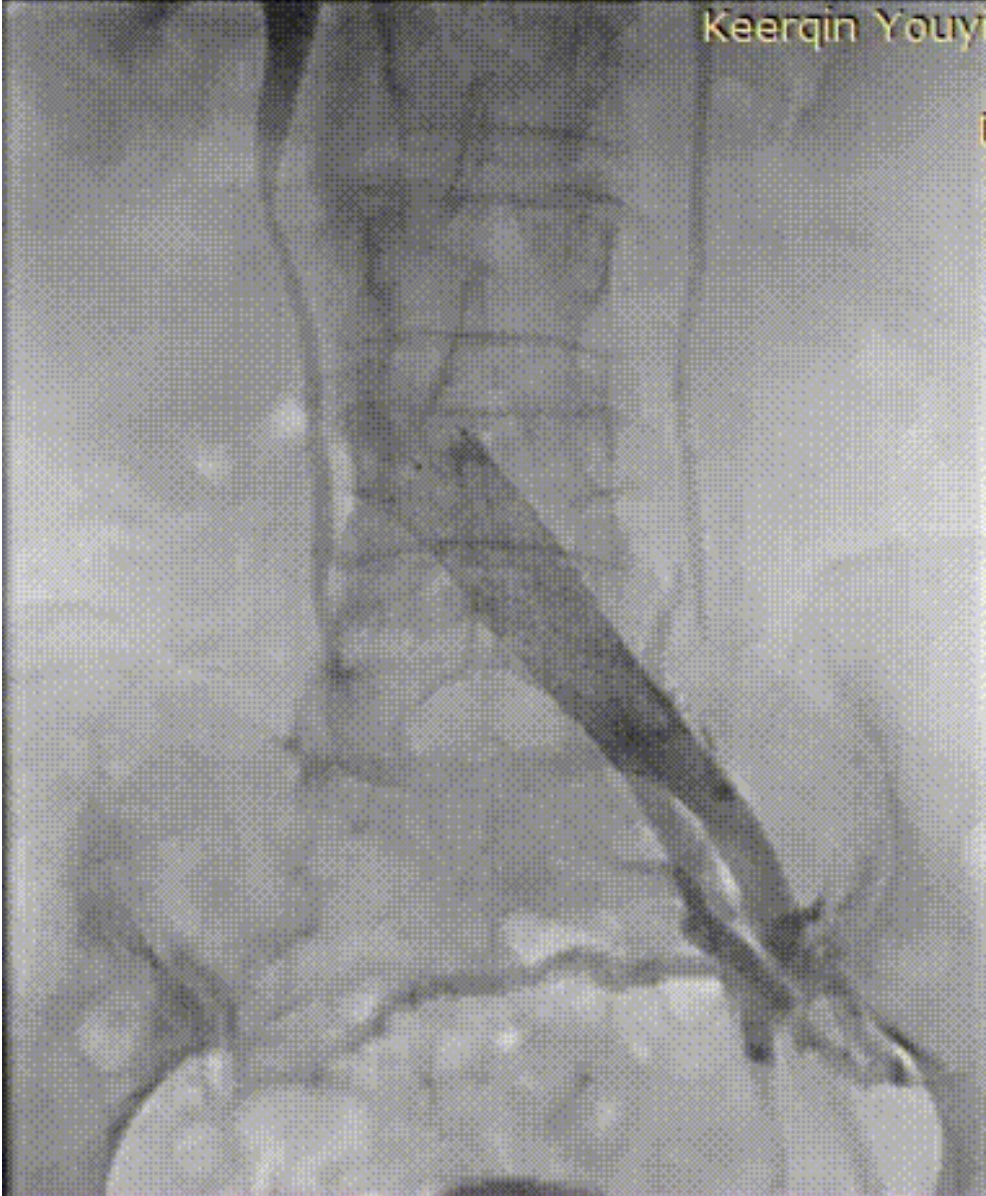
6) After posterior dilation, the common iliac vein stenosis disappeared, the blood flow was smooth, and the left to right shunt of the iliac vein was significantly less.
7) Subsequently, left great saphenous vein high ligation and exfoliation + punctate exfoliation of superficial varicose veins below the knee.
Postoperatively
6. Follow-up needs and doctor's instructions
1) Postoperative anticoagulation, swelling and pressure therapy.
2) Rivaroxaban tablets 20mg qd.
Postoperative summary
7. Summary of the operation
1) The patient was admitted to the hospital due to varicose veins of both lower limbs with soreness and skin ulceration, and was confirmed to have left iliac vein compression syndrome after enhanced CT examination and preoperative DSA imaging, and bilateral saphenous varicose veins of the lower limbs, and left iliac vein balloon dilation stent implantation, high ligation and peeling of the left saphenous vein + punctate decortication of superficial varicose veins under the knee. Venovo intravenous stent was used during the operation, the surgical effect was good, the patient could recover after surgery, no complications were seen, and a long-term drug + pressure treatment regimen was given.
2) Cockett syndrome is another important factor that causes varicose veins, swelling and pigmentation of the lower limbs in addition to primary varicose veins of the lower limbs.
3) Conditional centers can choose to use intraluminal ultrasound during surgery, which is more intuitive to evaluate the lumen stenosis before and after stent implantation.
4) Repeated comparison of the anatomical position and bony markers of the stenosis during the operation can provide more accurate positioning of the stent.
5) The duration of postoperative anticoagulation depends on whether there is thrombosis, if it is acute thrombosis combined with Cockett syndrome, anticoagulation often needs to be longer than that of patients with Cockett syndrome alone.
Expand the discussion
1. Patients with iliac vein compression syndrome should be treated with anticoagulation and compression stockings at the same time as swelling reduction treatment.
2. For varicose veins with Cockett syndrome, the sequence of varicose vein surgery and iliac vein stent implantation and whether it is necessary to perform surgery at the same time are still controversial. Some scholars believe that iliac pressure is the cause of varicose veins, so it is necessary to solve the compression before the varicose veins can be completely relieved, and even some scholars believe that iliac vein stent implantation can be performed simply first; The opposing voice believes that iliac pressure is not necessarily the cause of hemodynamic abnormalities, and the problem of blood reflux in the lower limbs is solved by varicose vein surgery first, and the patient's symptoms will be significantly alleviated after varicose vein surgery, thereby reducing the stent implantation rate. However, there is a lack of literature to support this view.