Speaker: Andrey Ivanov, MD
Institution: Medservice Hospital, Salavat, Russia
Abstract
This article presents a rare case of prostate cancer with concurrent May-Thurner syndrome, highlighting the therapeutic strategy for combined oncologic and anatomic venous compression. Leveraging the technical strengths of the Venovo Venous Stent (BD) and the innovative design of Boston Scientific’s Athletis Ultra-High-Pressure Balloon, this study provides clinical insights and research implications for managing complex iliac vein obstruction.
Introduction
Iliac vein obstruction arises from diverse etiologies, including tumor compression or May-Thurner syndrome (iliac vein compression syndrome). Patients often present with refractory limb swelling and pain, resistant to conservative management. Imaging-guided endovascular interventions, particularly bifurcated stent techniques (V-stenting), have emerged as critical solutions for restoring hemodynamic stability, especially when oncologic and anatomic pathologies coexist.
Case Analysis: Precision Application of Bifurcated Stent Technology
Patient Profile
Age and Presentation: 62-year-old male with chronic severe right lower limb edema, unresponsive to conservative therapy.
Medical History: Prostate cancer (T3aN0M1b) with multiple bone metastases, right hydronephrosis (Stage II, nephrostomy in August 2023).
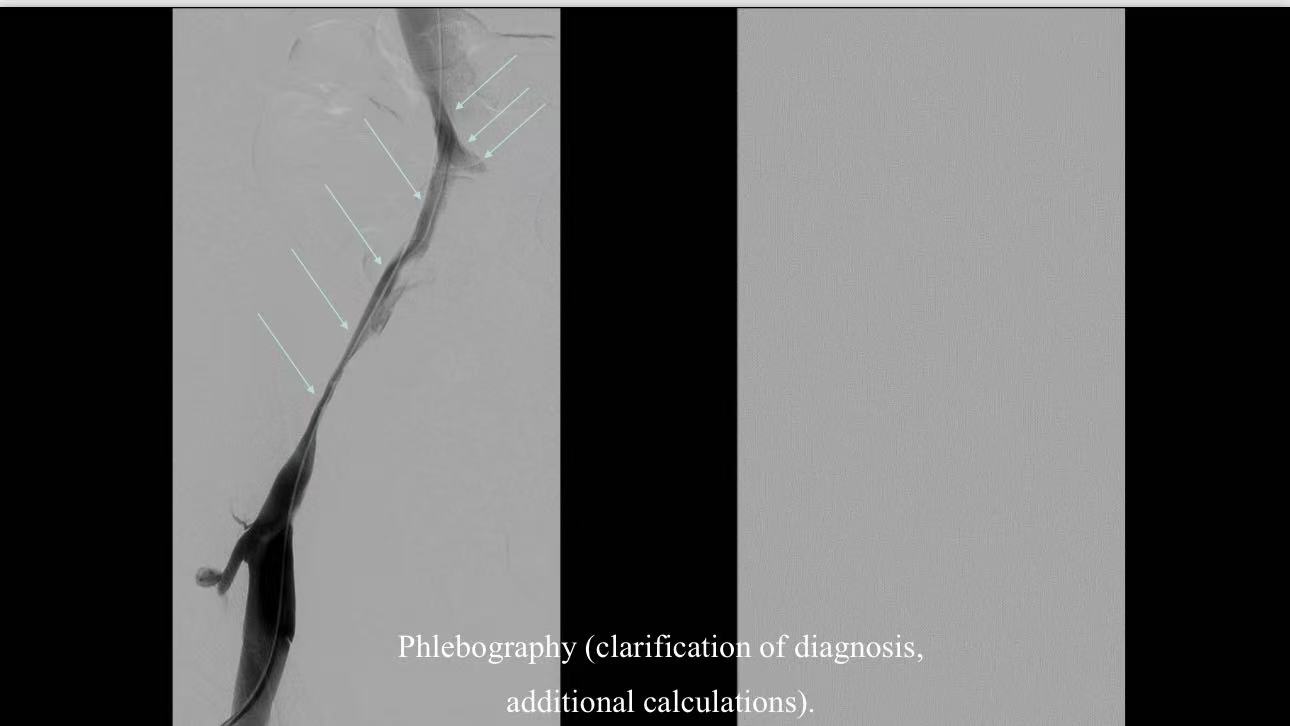
Imaging and Diagnosis
CT Findings:
Severe tumor compression of the right common and external iliac veins.
Concurrent May-Thurner syndrome (distal IVC and left common iliac vein compression).
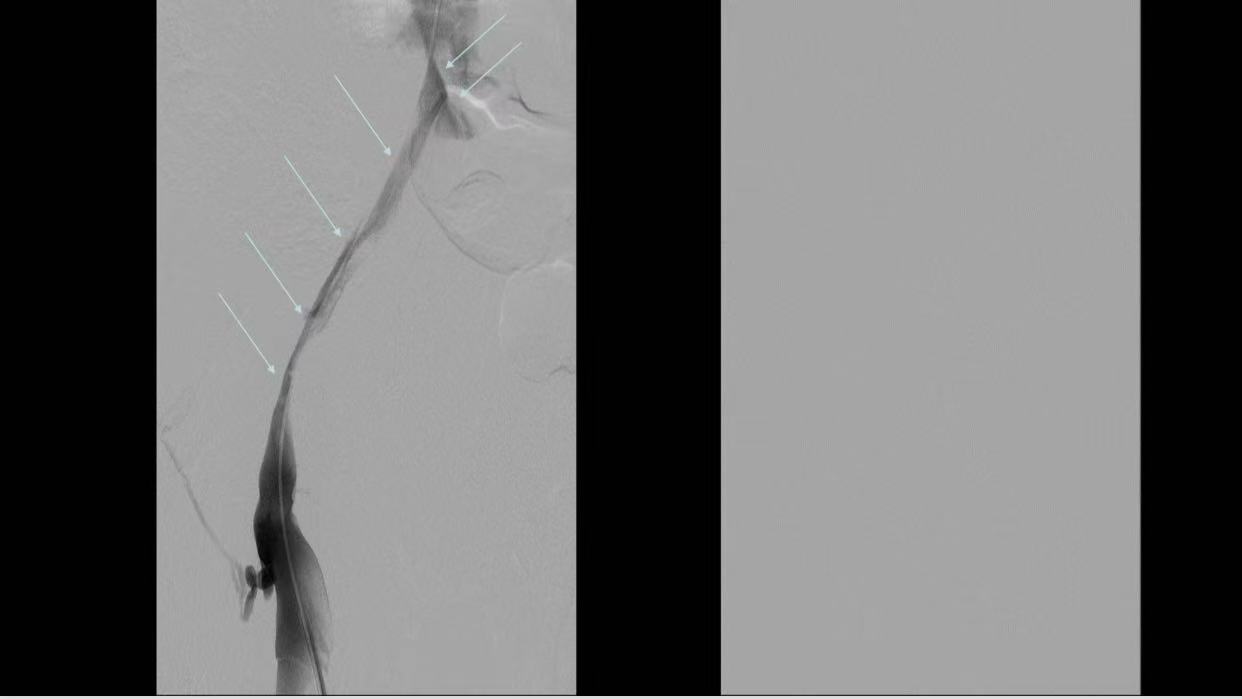
Venography: Extensive collateral circulation with significant elastic recoil in the right iliac vein.
Therapeutic Challenges
Unilateral stenting (right iliac vein) risked exacerbating contralateral thrombosis.
Requirement for bilateral compression relief and hemodynamic stabilization.
Surgical Strategy and Device Application
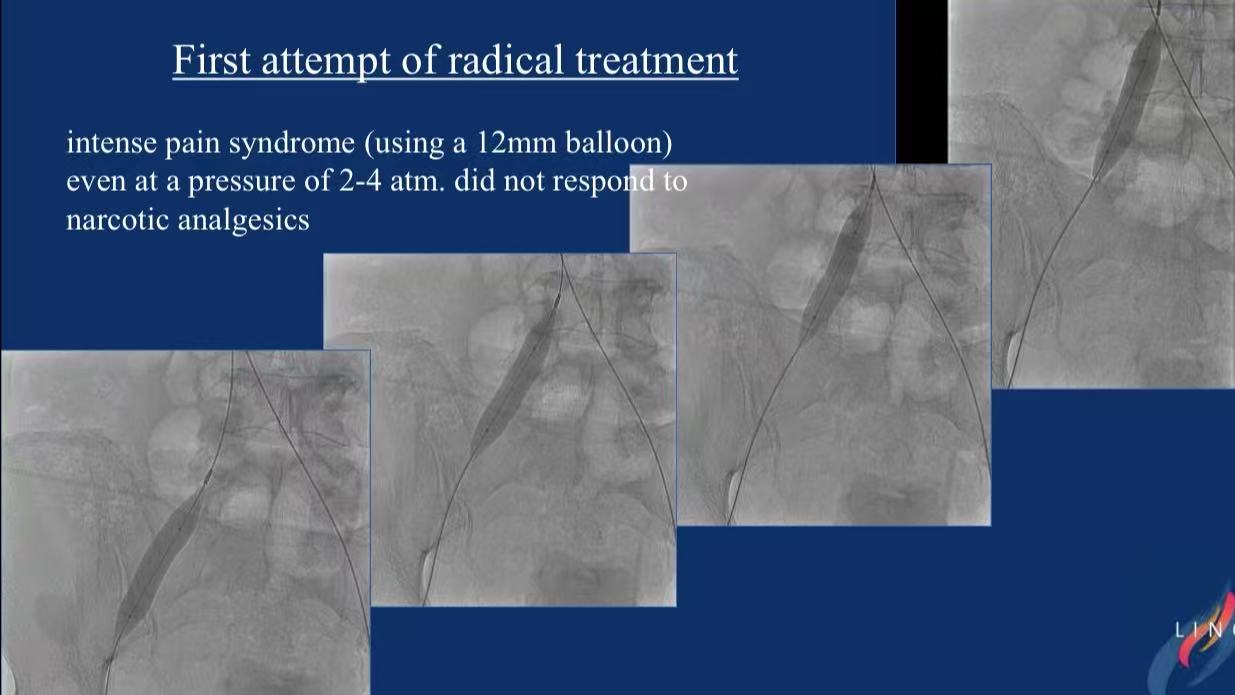
1.High-Pressure Predilation: 12mm and 14mm balloon angioplasty (hypothetical use of Athletis Balloon for resistant lesions).

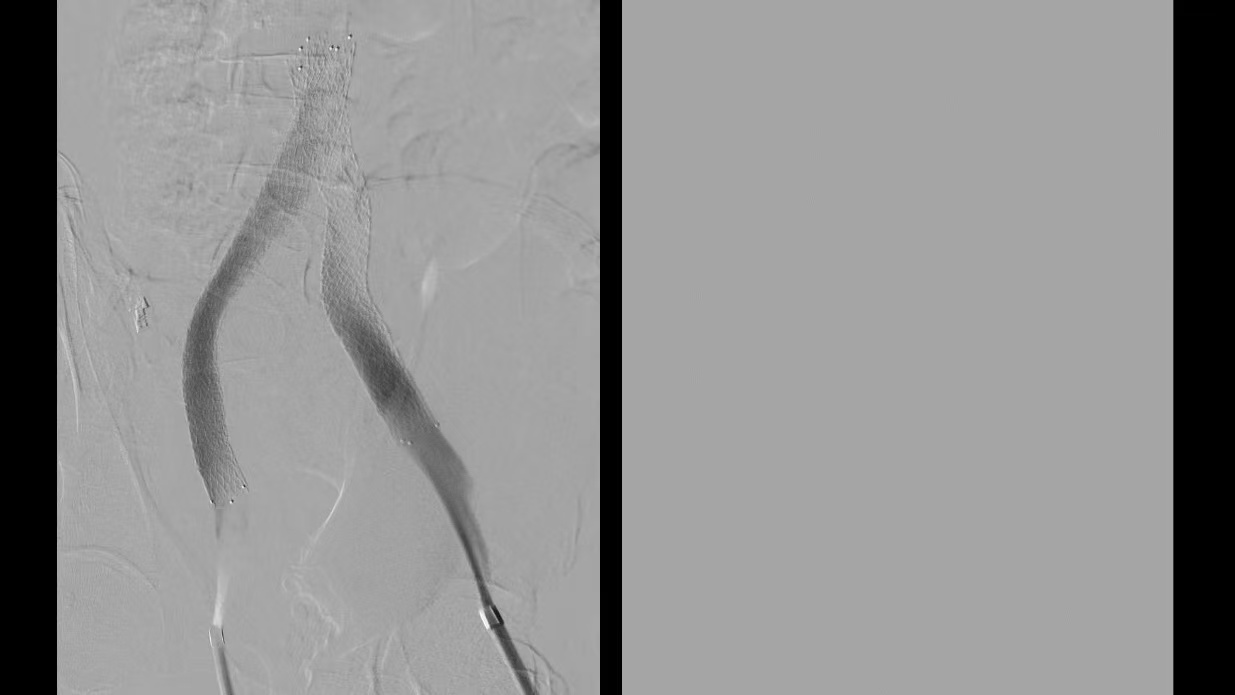
2.Bifurcated Stent Placement:
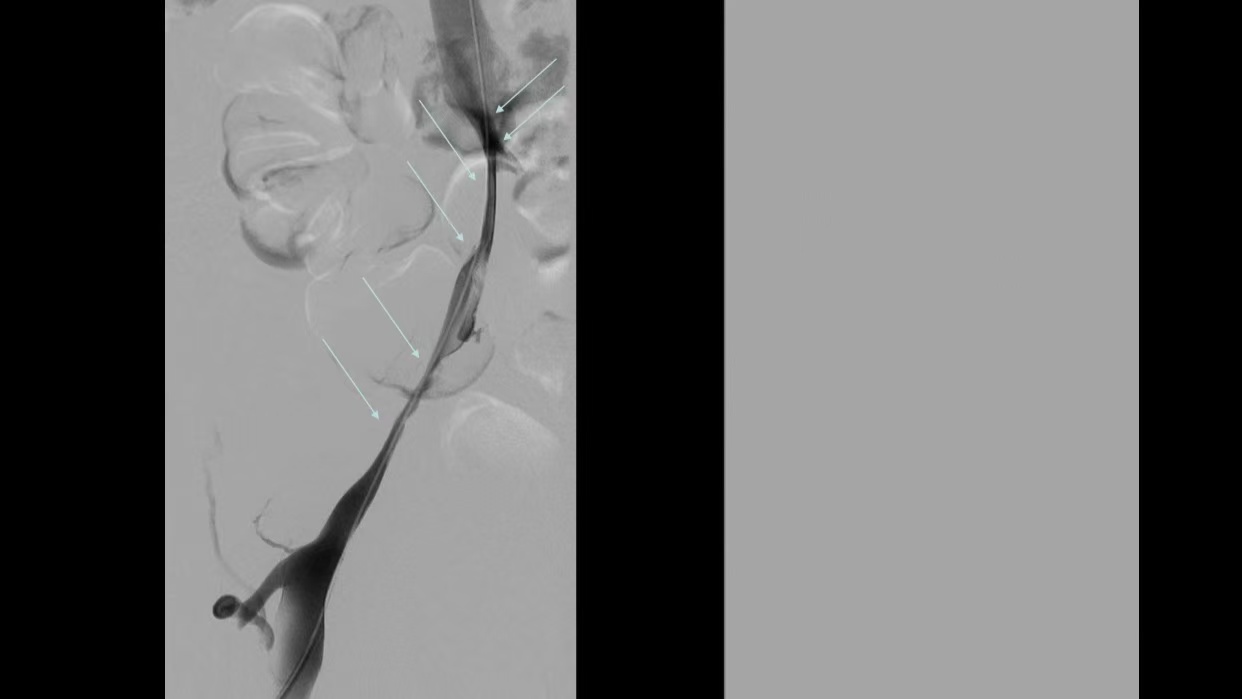
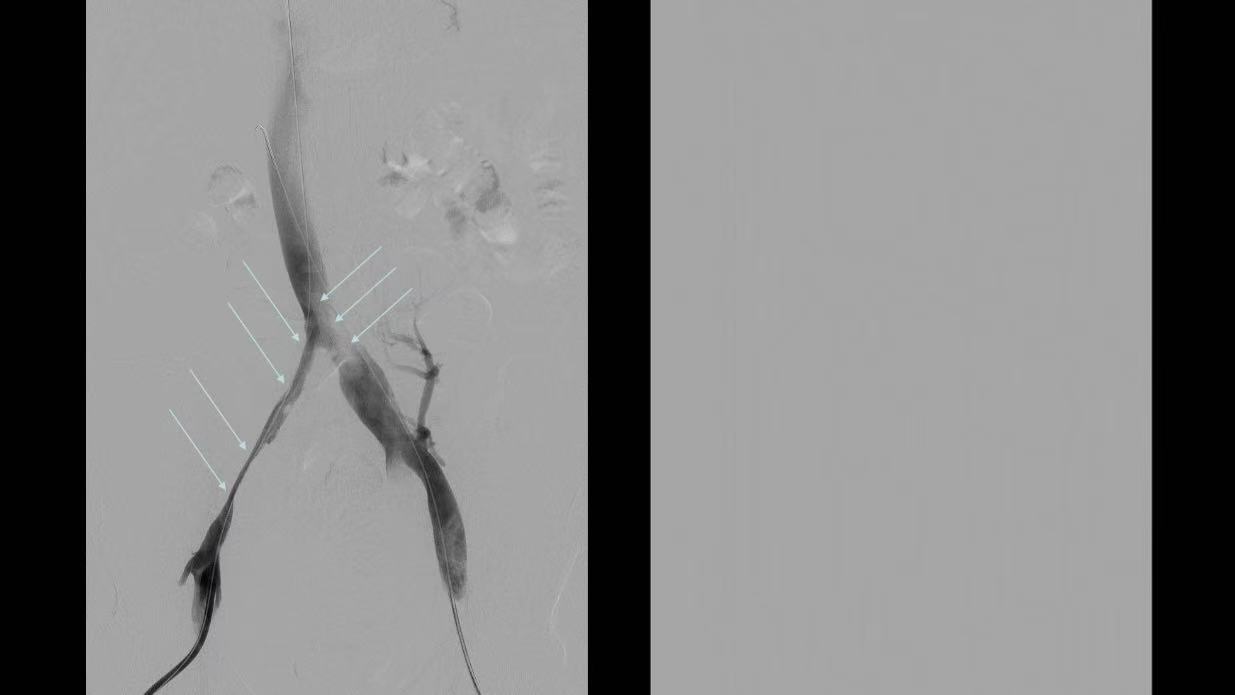
V-stenting under general anesthesia to cover bilateral lesions.
Flared ends and tantalum markers for optimal apposition and fluoroscopic guidance.
Dual-speed triaxial delivery system for precise deployment at the iliac orifice.
Device Selection: Venovo Venous Stent (BD, 14×160mm and 14×140mm).
Technical Details:
Outcomes
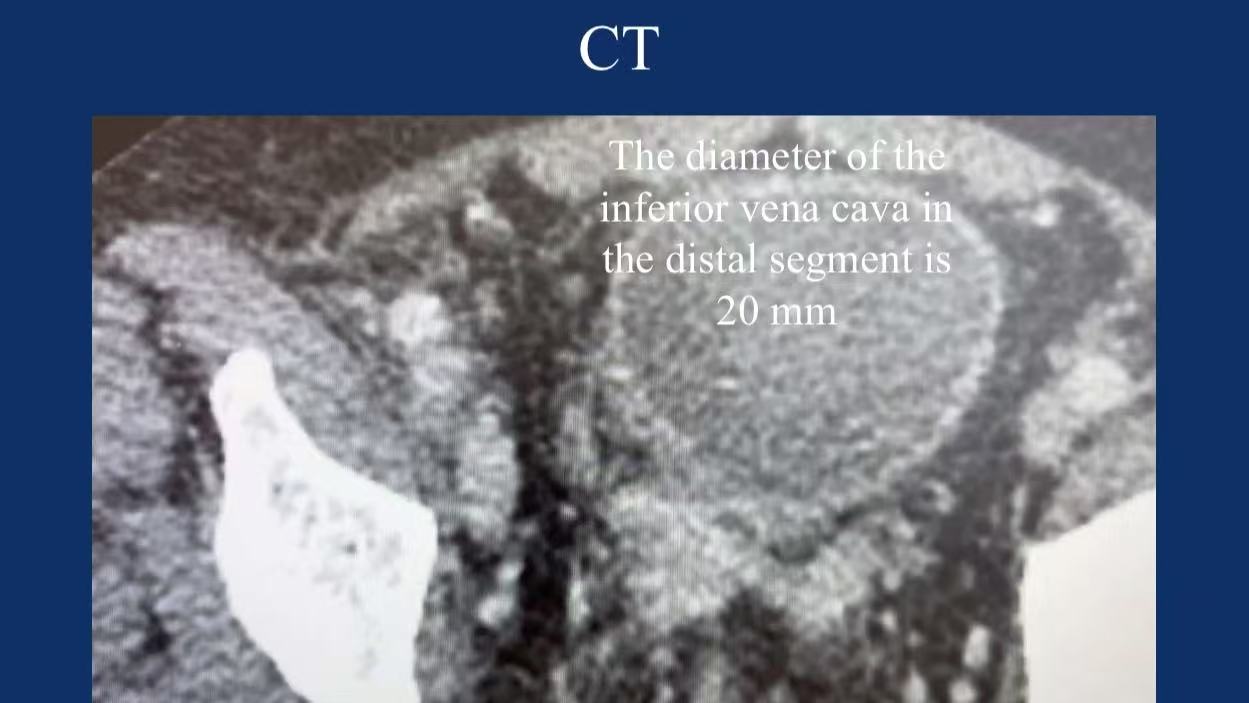
Imaging Confirmation: Distal IVC diameter restored to 20mm, complete bilateral decompression.
Clinical Follow-Up: Discharge on day 6 with resolved swelling and pain; no recurrence at 6.5 months under anticoagulation.
Product Innovations: Synergy Between Venovo Stent and Athletis Balloon
| Feature | Clinical Value |
|---|---|
| Venovo Stent | |
| - Radial Strength | Composite mesh design resists tumor/anatomic compression (95.5% primary patency at 36 months for NIVL subgroup). |
| - Anti-Migration | Tantalum markers and flared ends enhance visibility and wall apposition. |
| Athletis Balloon | |
| - 40ATM Ultra-High Pressure | Woven balloon technology addresses calcified/fibrotic stenosis (critical for predilation in resistant cases). |
| - Low-Profile Tip | 0.042-inch tip penetrates severe stenoses while minimizing vascular trauma. |
Conclusion
Necessity of Bifurcated Stenting: Dual pathology (tumor + May-Thurner) mandates bilateral hemodynamic assessment; V-stenting mitigates contralateral thrombosis risks.
Innovative Device Integration: The Venovo stent’s balance of strength and flexibility, combined with ultra-high-pressure balloon predilation, offers a comprehensive solution for complex iliac lesions.
Multidisciplinary Collaboration: Tailored strategies require coordination among oncology, interventional radiology, and vascular surgery to optimize oncologic control and vascular recovery.